Enabling transformation in health care quality
Executive summary
Change management is the process, method, and manner in which an organization identifies, defines, approaches, socializes, and implements significant change within internal and external environments. This includes preparing and supporting employees, establishing the necessary steps for change, and monitoring pre- and post-change activities to ensure successful implementation.
The need for change can be triggered for various reasons, some of which allow for controlled change and others where circumstances drive forced change. Crises such as COVID-19 present the most recent example of forced change which has had broad impact on many organizations. The natural life cycle of hospitals include leadership and/or regulatory changes which also present many opportunities for managing change. In fact, mergers and acquisitions have been a primary driver of change in the hospital setting since 1990.
In a recent partner survey, Q-Centrix found that 67% of partners had considered a significant change within their environment: centralizing. However, only 45% of respondents completed their centralization efforts. Among those respondents who had considered but not completed the effort, the majority indicated that the reason they did not execute on the strategy was due to a lack of understanding of the process to achieve the centralization. In fact, hospitals indicated they lacked adequate change management to successfully achieve their changes.
Without adequate change management strategy, health care providers who embark on visionary change, like centralization, are prone to less-than-optimal results. Many hospital systems fail to adapt to the “white waters” of change. The white-water rapids metaphor is often used to illustrate change in an environment which may lack stability and predictability and requires managers and organizations to actively and continually adapt to change. Without continuous “changing” and adaptation to ensure long term viability, Harvard Business Review notes, “70% of change management solutions ultimately end in failure.”
67%
of partners had considered a significant change within their environment: centralizing.
45%
completed their centralization efforts.
70%
of change management solutions ultimately end in failure.
Findings
- Transformative change management offers hospital systems greater agility and a more defined, collaborative, process.
- When following best practices, transformative change management results in higher rates of success when compared to traditional methods, with up to 79% of those taking a transformative approach reporting successful change management.7
- No single best practice can ensure successful change management, all best practices should be considered and implemented after careful consideration.
- Change creates a permanent “white water” that continually evolves. The management of change should therefore be ongoing, rather than a single instance or exercise.
Conclusions
Given the benefits and high rates of success in implementing lasting change, it is paramount that hospital systems undertake a transformative approach to their change management to successfully achieve their goals. When high levels of communication, collaboration, adaptability, and accountability are engaged, transformative change management can help facilitate a stable and sustainable change.
Defining transformative change
Generally, change management methods are one of two types: traditional and transformative.
Traditional change
Traditional change management is linear and “laned.” This method is often filled with heavy oversight management and rigid roles and can result in slow problem resolution. This method often focuses on returning situations to the status quo after major changes or crises (such as COVID-19).
Transformative change management
Transformative change management focusses on a vision. This method anticipates the indirect path of change and incorporates flexibility into the process, welcoming feedback and adjusting accordingly. Companies such as Deloitte note that this type of change is “agile”. Transformative change management solutions have been found to have a 79% success rate, compared to a 70% failure rate with traditional change management solutions.
Transformative change and Rapid Cycle Improvement Process
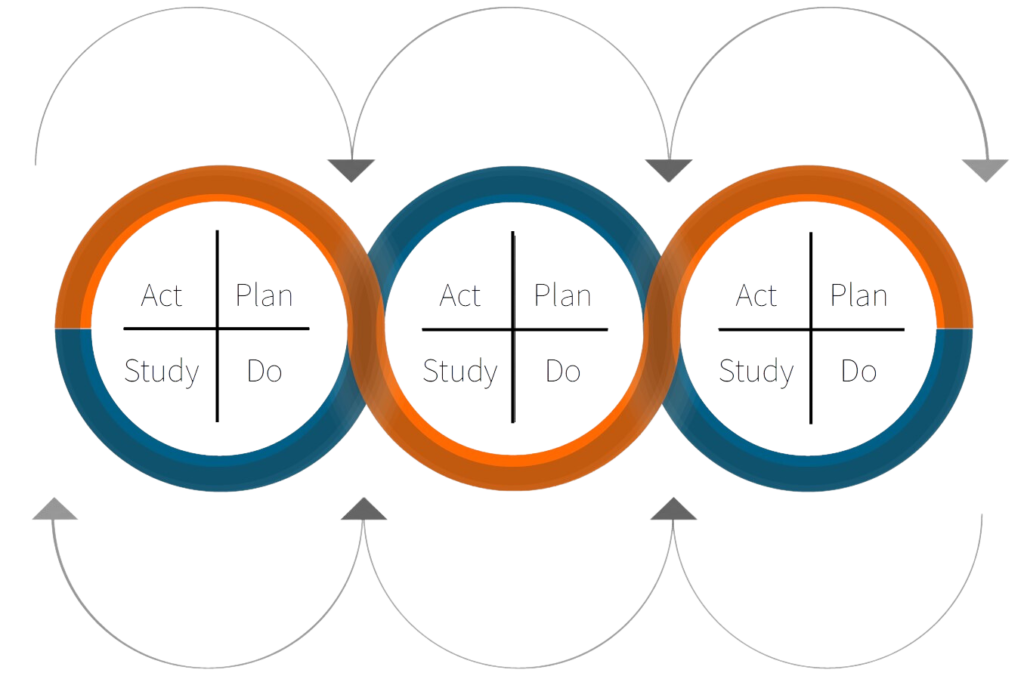
Transformative change management’s high rates of success is often attributed to its focus on a collaborative and agile process. The Rapid Cycle Improvement Process (RCIP) is a strategy used by Q-Centrix partners to quickly introduce change in increments leading to Transformative Change.
The RCIP is, a “quality improvement method that identifies, implements and measures changes made to improve a process or a system quickly. Rapid cycle improvement (RCIP) implies that changes are made and tested over a short period of time — cycles of three months or less rather than the standard eight- to twelve-month process.”
A successful RCIP will:
- Identify and Plan: Isolate desired improvement (need for change) and plan a change test (pilot)
- Do: Execute the plan on a small scale first and gather the results (before, during and after)
- Study: Examine the results to determine if they achieve desired results
- Act: Decide next steps. If desired results were not met, adjust plan as needed and repeat the process until desired outcome is achieved. If change is successful, implement on a larger scale.
Repeat: Begin new cycle. Continuously seek feedback and improvements throughout the process from individuals, senior leadership and affected departments. Enact the changes, adjust based on feedback or results, and repeat the process as needed.
Best practices in transformative change management
Define the change vision
Define the vision and identify the timeline of the change. Will this be a temporary, permanent or continuous change? Explain the process and how you seek to involve appropriate team members’ feedback to achieve the vision.
Pursue sustainable change
Healthcare is in a continuous process of innovation to ensure excellent patient care, market competitiveness, and financial growth. Therefore, introducing an added change can easily result in an unpleasant work environment. Define a vision that results in sustainable change based on the unique factors of your environment.
Establish the need for change
It is critical to establish and reiterate the need for change early in the process. While different audiences may be motivated by different goals, recent research indicates that incentives for a better and more engaging workplace structure is an attractive goal to most. Consulting firms such as McKinsey note that, “while momentum for change takes time and effort to build, once employees become excited or buy in to the goals of change it is, hard to stop.”
Communicate and socialize the change goals
Identify key stakeholders that will influence and inspire the change needed to achieve it.
Engage these leaders by explaining mutually beneficial goals that lead to the new vision. Then, assign accountability of each change milestone to a key stakeholder. These individuals will support continuous feedback during the change process and own the communication for each milestone. He or she will seek to understand feedback and resolve concerns prior to milestone achievement and afterward. This socialization process will facilitate the adaptation of change and engage a larger audience.
Seek objective perspective on the change
Bias can often blind internal stakeholders to the pitfalls of the process, timeline, goals or vision. Similarly, a fresh perspective may identify opportunities for efficiency. Therefore, it’s best to seek unbiased perspective on your plan from individuals who are not impacted. In larger, complex change processes, an expert external evaluation is ideal to ensure the plan is complete.
Prioritize changes
In any complex change process, there will be multiple changes. Some change can be executed quickly while other changes may have prerequisites or require a longer feedback process prior to implementation. Facilities embarking on a change process should identify each change and designate them by priority, type of task, and resources required to complete. Completing different change items early or later in the process will prevent teams from being overwhelmed with too much change and will help ensure a smooth and sustainable transition.
Conclusion
Change can be triggered by the natural life cycle of a hospital system or by a global pandemic such as COVID-19. Regardless of the catalyst for change, the process by which you implement change will have a significant impact on its success. Transformative change management focuses on a collaborative and agile process that establishes clear lines of communication and accountability. In addition to incorporating the RCIP into the process, other key attributes of transformative change include identifying the need, defining the vision, pursuing sustainable change, communicating and socializing the change, seeking objective perspective, and prioritizing changes.