Navigating the health care labor shortage and its effects on clinical data management
Introduction
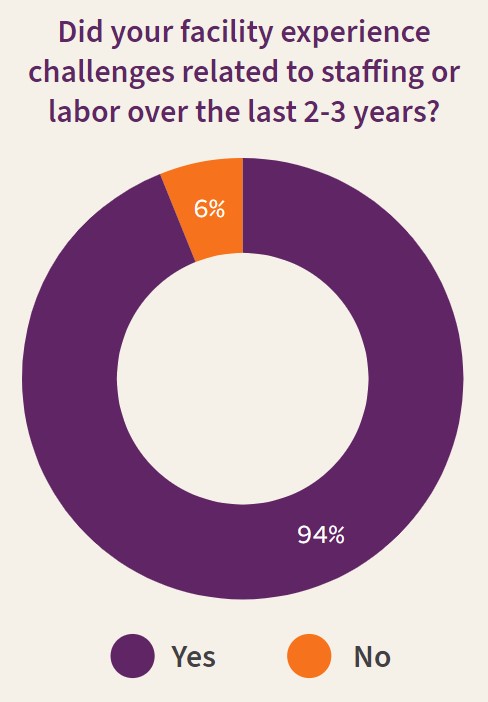
The health care industry is facing a critical staffing shortage. Between February and June 2022, more than 2.7 million health care and social assistance workers quit their jobs — and hospital executives are already feeling the effects of these departures. In a 2022 Q-Centrix survey of hospital quality leaders, more than 90 percent of respondents said their facility experienced challenges related to staffing or labor in the last two to three years.
This health care staffing shortage is expected to persist well into the coming years. Estimates show that by 2026, there will be a lack of 3.2 million critical health care workers (e.g., medical assistants, home health aides, and nursing assistants) and 1.1 million nurses. Physicians will be in short supply as well, with an anticipated shortage of between 37,800 and 124,000 physicians by 2034.
While much is known about some impacts of the labor shortage, a less discussed consequence concerns data. Clinical data are key to countless hospital operations, including monitoring patient safety, identifying gaps in care, and measuring hospital performance. Because these data have immense untapped potential to help health systems improve patient care, there is a great need to understand how the shortage affects clinical data practices.
To learn more about the labor shortage’s impacts on clinical data management, Q-Centrix administered a survey to its partners in July and August 2022 and held a small group discussion with hospital leaders. This white paper shares findings from this research, explores how the shortage affects clinical data management practices and staffing levels, and discusses possible ways for hospital executives to address these effects.
Causes of the labor shortage
Impending retirements
Baby boomers comprised the largest living generation in the U.S. until 2019. With all baby boomers set to reach age 65 or older by 2029, their retirements are expected to leave major gaps in the workforce. Projections indicate that the percentage of primary care physicians reaching retirement age will climb from 12 percent in 2021 to 21 percent in 2026, and more than one-fifth of nurses are planning to retire from nursing by 2025.
Aging population
An added consequence of this aging population is an increased demand for health care services, another driver of the shortage. Older people are more likely to have multiple diagnoses and comorbidities, which necessitate health treatment.
COVID-19 pandemic
The COVID-19 pandemic has been linked to an increase in retirement among U.S. adults ages 55 and older, suggesting that some older adults may be retiring even sooner than anticipated. Further, health care workers have experienced heightened burnout as a result of the pandemic, causing them to leave the profession in greater numbers.
Impacts on clinical data management
Many impacts of the labor shortage are widely known. With fewer staff available to administer care, patients may be at risk of higher rates of infections and medical errors, as understaffing is associated with an increased risk of health care-associated infections. Additionally, working at understaffed hospitals is taking its toll on health care workers, leading to high levels of stress, low job satisfaction, and burnout. Hospital executives are already seeing impacts on their budgets: hospital labor expenses have risen by more than one-third compared to pre-pandemic levels, owing to labor shortages and the increased reliance on contract workers.
Much less is known about how the labor shortage affects clinical data management. Health care leaders struggling to maintain sufficient staffing levels may lack the resources to devote attention to other areas, such as capturing and interpreting clinical data to inform decision-making, improve outcomes, and support regulatory compliance.
To learn more, Q-Centrix gathered insights from hospital executives, both through a small group discussion with hospital partners and by fielding a survey of hospital quality leaders in July and August 2022. These findings, cited throughout this white paper, revealed the extent to which the shortage has impacted clinical data management practices and staffing levels.
Clinical data management and affected service areas
Nearly nine in 10 respondents said labor challenges changed how they managed their clinical data. Less than 15 percent reported that labor challenges had no change on how they manage clinical data.

When asked about specific areas impacted by labor challenges, clinical data executives were most likely to see impacts in the quality of care delivered. Many respondents also mentioned seeing impacts in more than one area. Likewise, discussion with Q-Centrix’s hospital quality partners revealed that maintaining adequate staffing across multiple service areas has been a challenge. One partner shared that due to turnover among their improvement advisors, they had to find ways to shift staffing without neglecting any service areas: “[We had to] reevaluate not only our data resources, but our improvement resources to make sure that we were really hitting those service areas that had a lot of weight—but also not leaving the service areas behind that didn’t have an improvement advisor just because of the lack of staffing.”
Staffing and hiring
Two-thirds of respondents reported seeing impacts on clinical data management staff at all levels. This may be why some hospital executives have changed their hiring practices to bring in staff with less experience. “We always used to take on . . . experienced nurses. That’s our pool generally, and that’s gotten tougher,” said a hospital partner. “We’re actually being encouraged to really think outside that box. So I think we’re trying to bring younger, less experienced people on, who maybe have a little bit of a tech side to help with some of the reporting as well, to really look at this data fully.”

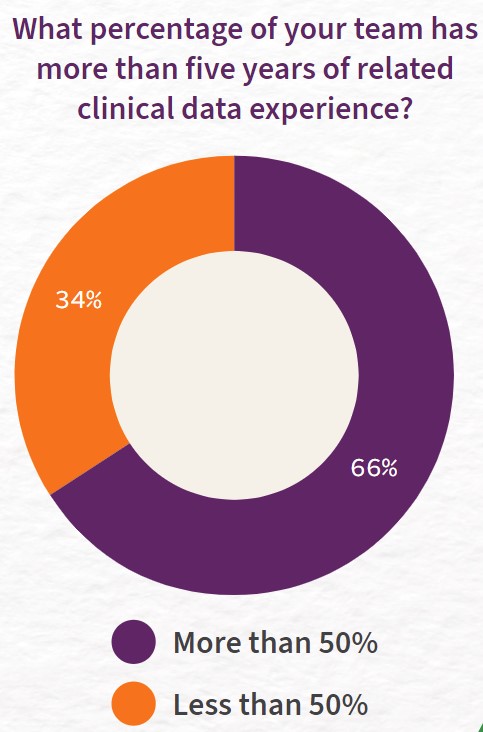
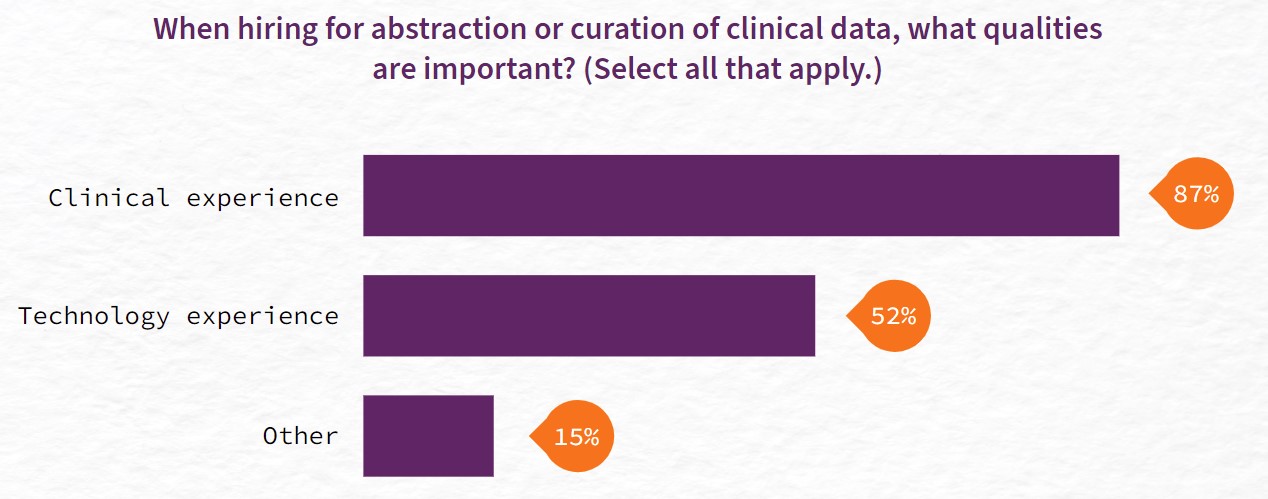
Q-Centrix’s survey confirmed this trend: about a third of respondents reported that less than half of their team had more than five years of clinical data experience. This does not mean, however, that leaders do not value this experience. About nine in 10 survey respondents cited clinical experience as an important quality for abstraction or curation of clinical data, while just over half valued technology experience. The remainder listed other skills, such as attention to detail, abstraction experience, or critical thinking skills. However, hospital leaders may not be able to hire staff with all the skills and experience they desire. Instead, they may need to train less experienced staff to fill in knowledge gaps.
While hospital partners cited hiring staff with less experience as a tactic to contend with the labor shortage, they explained that this requires an added time commitment. “Our team was already stretched thin to the brink,” said one hospital partner. “To bring someone in that we would have to fully train from the ground up, we knew it would probably take 50 percent away from their normal responsibilities.”
Looking ahead
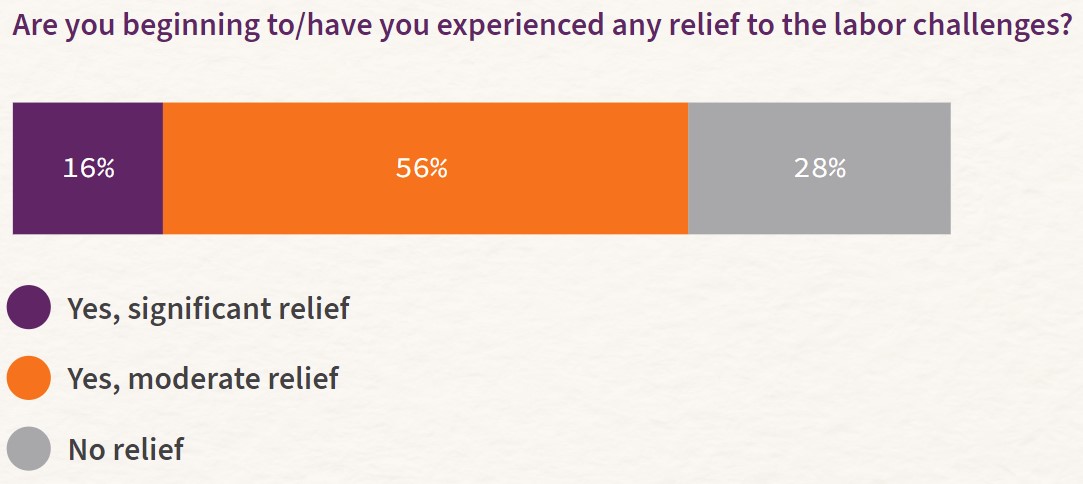
Despite these challenges, good news is on the horizon. Nearly three-quarters of respondents said they have begun to see relief from the labor challenges. However, more than a quarter reported that they have not experienced any relief, suggesting that some hospital leaders will continue to face difficulties ahead.
Strategies to mitigate health care staffing shortages
Take action to alleviate and prevent burnout among health care workers
Burnout among health care staff can have devastating effects, including lower quality patient care, medical errors, risk of malpractice and increased costs for health care systems, and worsening public health outcomes.20 Some measures hospital executives can take to help prevent burnout include fostering a culture of teamwork and open communication, increasing access to mental health and substance abuse care, and reducing administrative burden on health care workers.
In a discussion Q-Centrix held with hospital partners, one leader shared that they implemented an employee wellness program to encourage staff to prioritize their well-being. Another partner added employee wellness to their hospital’s clinical scorecard goals. “We actually added in a dimension called caregiver well-being,” the partner explained. “So we have measures tied to it. We were actually able to put some data behind it, and measure it, and actively try to improve that.”
Conduct an assessment
With growing labor expenses and rising inflation, hospital executives will need to take stock of their spending and find ways to cut costs. For example, Q-Centrix estimates that a health system with eight to 10 hospitals spends an average of $6 million to $8.5 million on clinical quality data every year. These costs are often fragmented across several different hospital budgets, making it difficult to discern how they add up across the entire health system. By conducting an assessment, health systems can gain a better understanding of their clinical data spending and receive guidance on how to improve efficiencies.
“The assessment is a tool by which we provide a focused analysis that highlights what the true costs are and how to better align operations to high-value activities and reduce costs,” explains Doug McGill, lead consultant for Q-Centrix Advisory Solutions. “When 80 percent of the costs of clinical quality data operations are tied up in people, it’s critical that you have staff performing at the highest impact.”
Use technology or automation to mitigate challenges
Leveraging emerging technologies such as artificial intelligence (AI) platforms has been recommended as a critical strategy for mitigating the staffing shortage. AI platforms can be powerful tools in providing clinicians with the data they need, aiding in clinical decision-making, and reducing the administrative burden on clinicians.
Findings from Q-Centrix’s survey and discussions with hospital partners confirm that many hospital quality leaders are turning to technology. “Definitely within the last year or two, we’ve put in more requests to have more of our data automated,” explained a hospital partner, noting that they especially look to automate projects that are time-consuming. Similarly, Q-Centrix’s survey found that 36 percent of respondents reported that they employed technology or automation to mitigate challenges presented by the labor shortage.
Partner with a third party
Third-party partnerships can ease the burden on short-staffed health systems, allowing overworked staff to focus on areas where they are needed most. As a report from the U.S. Department of Health and Human Services explains, “Technology companies can ensure that patient-generated data is accessible in a meaningful way and does not result in increased burdens on health workers.” Many hospital quality leaders have taken this approach: Q-Centrix found that labor shortage challenges have led more than a third of survey respondents to increase the scope or volume of third-party partnerships they use.
According to a leader at a health care system that has been partnering with Q-Centrix since 2016, having third-party help prior to the pandemic helped them be as prepared as possible when they started to feel the effects of the labor shortage: “I think it’s been really helpful as both a partnership and a safety net. Having the depth of expertise with people who do this work full-time.”
Allocate time for training.
With the shortage driving hospital leaders to hire employees with less experience, training is key to ensuring these staff have the skills they need to excel in their roles. A hospital partner revealed that cross-training—which involves teaching employees how to perform job functions outside of their role—has been a valuable strategy during the shortage. “I think cross-training and making sure that everyone has a backup—it’s definitely been our biggest lesson learned,” the partner said. A benefit of cross-training is that it can help organizations maintain productivity during workforce shortages.
Another hospital partner shared that while hiring less experienced staff for clinical data management involves more training, these employees can bring a useful perspective to the team. “There is an objectivity that a non-clinician brings to this work that is very valuable,” the partner explained. “They require a different type of training than a clinical person does, but they bring a different benefit to the team as well.”
Conclusion
While this shortage of staff in hospitals will continue to challenge the health care industry in the coming years, executives can take steps to lessen its effects on health care workers, patients, and their bottom line. Taking action now can help health systems prevent burnout, reduce administrative burden, and save on costs and staff time.