Meeting the new CMS health equity measures
An inside look at Houston Methodist's approach
Introduction
In August 2022, the Centers for Medicare & Medicaid Services (CMS) issued a final rule with three health equity-focused measures for inpatient and long-term care hospitals participating in its Hospital Inpatient Quality Reporting (IQR) program. As part of a larger initiative to advance health equity, these measures ultimately seek to ensure that all patient populations have a fair and just opportunity to attain their optimal health.
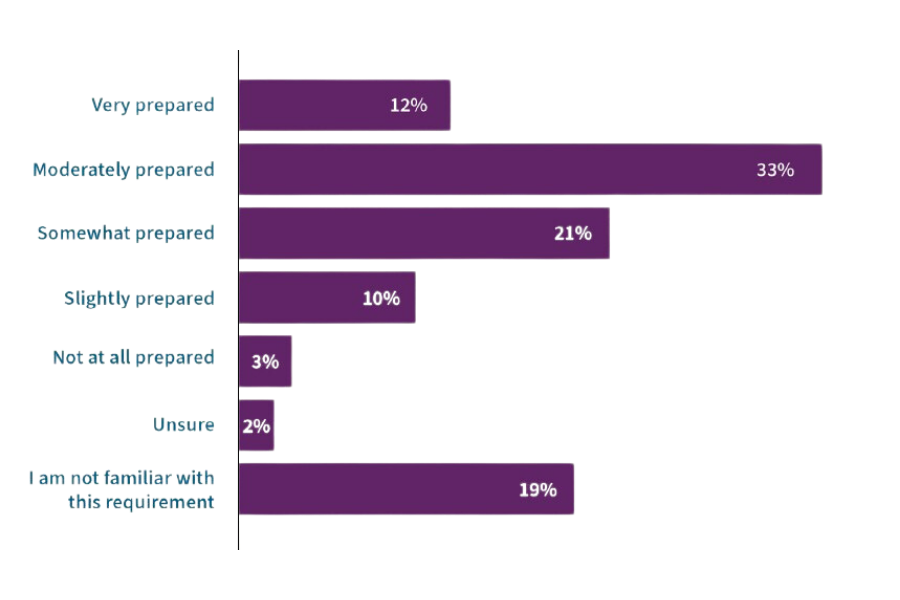
As a recent Q-Centrix survey of hospital and health system leaders showed, facilities vary widely in their preparedness for the new measures. When asked about their facility’s preparedness to meet the hospital commitment to health equity measure, nearly half of respondents felt their facility was very prepared or moderately prepared, and nearly a third said their facility was only somewhat prepared or slightly prepared. Another three percent reported that their facility was not at all prepared, suggesting that some hospitals are only just beginning their journey in advancing health equity.
How prepared is your facility or health system to meet the new CMS requirements for the Hospital Commitment to Health Equity measure starting in May 2023
Q-Centrix held a small group discussion with hospital leaders to learn more about their health equity efforts. One participant represented Houston Methodist, a Texas-based health system comprising an, academic medical center and six community hospitals. Houston Methodist has long been committed to equity. The health system’s Diversity, Equity & Inclusion (DEI) committee strives to maintain a culture of inclusive behavior and provide unparalleled care to a diverse patient population. When Pat Harrison, vice president of system quality and patient safety for Houston Methodist Health System, learned about CMS’s new health equity measures, she knew she would need to work with stakeholders throughout her facility to implement changes. With the first measure’s reporting period occurring in calendar year (CY) 2023—and the other measures transitioning to mandatory in 2024—Harrison and her team had to act quickly.
While preparing to meet the new measures continues to be an ongoing process for Houston Methodist, their experience so far offers a valuable example for hospitals and health systems that are working toward addressing the new health equity measures.
Health equity measures
The following three health equity measures from CMS encourage hospitals to build health equity into their core functions and address disparities in care:
Hospital commitment to health equity
This measure encourages hospitals to analyze data to deliver equitable care to Medicare beneficiaries and minority groups. The initial reporting period for this measure begins in CY 2023; participating hospitals must submit data on these domains for CY 2023 starting in May 2024. Participating hospitals will be required to attest to five health equity domains:
- Equity is a strategic priority
- Data collection
- Data analysis
- Quality improvement
- Leadership engagement
Screening for social drivers of health (SDOH-1)
Hospitals will be required to report the number of patients that are ≥ 18 years old and were screened for food insecurity, housing instability, transportation problems, utility difficulties, and interpersonal safety. Reporting for this measure is voluntary in CY 2023 and will be mandatory in CY 2024.
Screen positive rate for social drivers of health (SDOH-2)
Hospitals will be required to report the number of patients ≥ 18 years old who screened positive for at least one of the following: food insecurity, housing instability, transportation problems, utility difficulties, and interpersonal safety. Reporting for this measure is voluntary in CY 2023 and will be mandatory in CY 2024.
Taking action
Harrison’s first step in addressing the new measures was meeting with other departments to take stock and develop an action plan. Harrison’s quality team worked with leaders in DEI, case management, nursing, information technology, community benefits, training, and reporting. “We had three or four meetings in December and January to meet with leadership in other areas, because this takes a village,” said Harrison.
“We informed stakeholders about the domains and the screening tool,” said Dr. Keisha Whiting, DNP, senior quality outcomes specialist for Houston Methodist Health System. “Overall, we had to see where our leaders currently were, identify any gaps, and start seeing what we needed to do to get changes in place necessary for success.”
Overall, we had to see where our leaders currently were, identify any gaps, and start seeing what we needed to do to get changes in place necessary for success.
— Dr. Keisha Whiting, DNP, senior quality outcomes specialist for Houston Methodist Health System
Domain attestations
The hospital commitment to health equity measure comprises five domain attestations. Each domain is given one point for a total of five obtainable points across the domains. For domains with more than one element, facilities would not receive a point unless they met all elements in that domain.
The Houston Methodist team chose to be strategic when deciding which domains to focus their efforts on first. The two most natural starting points for Houston Methodist were:
Quality improvement
In addition to having just one element, the quality improvement domain—which states that the hospital participates in local, regional, or national quality improvement activities focused on reducing health disparities—covered activities Houston Methodist was already doing. “The fact that we are part of CMS Quality Reporting Programs would make this a yes,” Harrison said. “Moreover, we also have other national campaigns that our community health benefits department works on. We felt very comfortable saying that we could start here.”
Leadership engagement
The leadership engagement domain states that the hospital’s senior leadership annually reviews its strategic plan for health equity and key performance indicators stratified by demographic and/or social factors. Harrison felt Houston Methodist could comfortably address this domain given that its DEI committee was already active in the equity space. “We know that we are committed to DEI, and so our DEI department is going to be creating a letter of commitment, a plan, and presenting that,” Harrison said.
Above all, Harrison stressed the importance of reporting on the five domains, even for facilities that are not yet engaging in any of the activities listed in the domains. “Make sure you report, period!” Harrison said. “You do not have to be perfect on this.” Failing to report on this measure can automatically reduce a facility’s Medicare reimbursement rate by 25 percent. Regardless of how hospitals perform in each domain, they must provide an answer.
Social drivers screening measures
When addressing the social drivers screening measures, several steps proved useful:
Engage leadership.
“We engaged leadership across different departments to try to get more information,” Dr. Whiting said. “What is the current state? What are we currently screening for? Who is screening? What does that look like in our electronic health record? It is important to both research (within your quality department) and ask the questions throughout your system.”
Understand existing processes.
Dr. Whiting discovered that Houston Methodist’s case management team was already documenting details related to social determinants of health as part of their routine process and was working toward upgrading that process. Rather than develop a new screening protocol from scratch, the quality team found that it was more useful to draw from the processes and updates the case management team already had in place and look for ways to tailor them to the CMS measures.
Think through workflow considerations.
“We had to build [the screening tool] in the EHR, and where we built it drove who has access to some of these questions,” said Harrison. “It was important to decide what the workflow was going to look like. Take into consideration who may start asking the questions, and who may be able to complete the questions. This is also important to ensure that applicable follow-ups can occur related to answers from the screening.”
Leverage the health system’s EHR.
Houston Methodist’s EHR includes a wheel with social determinants of health (SDOH) elements. The Houston Methodist team plans to incorporate this into their screening tool process, as it indicates the completion of screening and provides multiple members on the care team with a visual representation of social needs. The EHR also has an upcoming upgrade that will simplify the reporting process and negate the need to report on SDOH needs manually.
Lean on resources for facilitating referrals.
“Companies such as Healthy Planet are a good resource for feedback related to needs,” said Dr. Whiting. “We also use a resource called findhelp (formerly Aunt Bertha). This provides by-zip-code information that can help patients align with different types of resources in the patient’s specific area for needs that may come from their screening tool answers. This further assists in allowing one to see how close or far the resource is from the patient in need.”
Collaborate across departments for training.
Harrison anticipates that training staff on the new screening process will involve multiple departments. “For the IT part, they have their own communication and training group,” said Harrison. “But they are going to have to partner with us and other stakeholders for some input and material. As this evolves, depending on what the final workflow is, registration could do part of it, along with nursing.”
Supplement training with video resources.
In addition to developing training materials in-house, Houston Methodist plans to use training videos from the Health Quality Innovation Network (HQIN). “The thing that is nice about the videos from HQIN is they are short and brief,” said Harrison. “Some are two to three minutes. You could ultimately QR code the video for quick review. If you are teaching a training and someone needs more information, you could say, ‘Here’s a QR code where you can watch this two-minute video now and if you need a refresher later.’” Dr. Whiting added, “This information has been shared with registration leadership for overall knowledge beyond the screening tool. The videos are useful for topics that some deem sensitive. This process started before this measure and will go beyond the measure. We want to be prepared for next stages and continue to serve our patients, their families, and persons significant in their life well.”
Pilot program
Goals
Houston Methodist is planning to conduct a pilot program with the SDOH screening processes in a few select units at the end of May 2023. This pilot enables them to:
Try out the new screening process and make adjustments.
“We have got to refer patients who screen positive to social work and case management as needed,” Harrison said. “What does that impact? We do not want to turn it on for a whole system, have them be slammed with requests, and then not be able to acknowledge or meet the needs of the patient. So, we are going to pilot the entire process on a couple of units and see what does that volume look like. Are we going to have to hire more social workers and case managers to meet the need to be able to do this? Or come up with some other solutions?” Dr. Whiting explained, “During the planning phase, discussion of screening tool answers needing consults versus discharge instructions was discussed with key stakeholders to attempt to meet the needs of the outputs from the tool. The pilot will allow further expansion on the pathway for answers provided to reach applicable sources.”
Ensure facilities are prepared to provide sufficient resources at all times.
“The screening has to be done in a timely manner to compile necessary resources,” said Dr. Whiting. “This includes on the weekend, and it includes if someone comes in Friday at 11:59 PM. To further expound on that, the same resources Monday through Friday during the day shift are sometimes not the same resources on a holiday weekend night shift. We are trying to ensure that we give all our hospitals the resources that they need for when someone does screen positive for something. During the planning phase, we have gone through the tool and aligned what needs a consult versus discharge resources with our case management department.”
Selecting units to involve
When deciding which units will be part of the pilot process, some considerations Harrison and Dr. Whiting cited include:
Interest from unit leaders
Harrison expects that some unit leaders will volunteer their department for the pilot. “We have some CNOs that are really early adopters, and they want to help you figure it out,” she explained. “They want their voice really heard in the process of what works and what does not work.”
Geographic and socioeconomic diversity
“We must consider that we have several hospitals in different geographical [and] socioeconomic areas that may have different needs and different available resources,” said Dr. Whiting. “We want to encourage all our hospitals to have a chance to go through the screening process on a smaller scale during the pilot phase.”
Planning for results and next steps
Houston Methodist expects to see results within about two weeks after the pilot. By this time, they should know the demand on case workers and be able to assess whether they need to hire more staff. Dr. Whiting noted that leadership has been kept informed about this possibility, ensuring they have leadership support to act on the results of the pilot and beyond.
“Overall information related to the health equity CMS measures was provided to our system leadership level early on in the process, and since [then], many updates [have been] provided. They are continually informed and are aware that there may be a need for additional FTEs.”
— Dr. Keisha Whiting, DNP, senior quality outcomes specialist for Houston Methodist Health System
With the pilot starting in the second quarter of CY 2023, Harrison anticipates that they should be able to start acting on the results of the pilot the following quarter. “At the beginning of the third quarter—so, July, August, September—we should be expanding this,” Harrison said. “We should have at least assessed it, and we should be hiring more people, or at least piloting on more units. Depending on each hospital’s resources, we should be able to expand it a little bit, and hopefully we will be able to optimize it.”
Lessons learned
Be strategic when deciding where to begin.
When Houston Methodist’s quality team was considering how to begin responding to the domain attestations, they focused on the quality improvement domain initially, as this domain aligned closely with their organization’s priorities. “Look for leverage in the five domains,” advised Harrison. “If you want a quick win, you can focus on [the quality improvement domain], which has only one element.”
Align with other departments.
Having regular meetings across departments to explain the new measures and develop a plan to address them helped Houston Methodist navigate change in a collaborative way. Dr. Whiting stressed the importance of explaining the reasoning behind the need for changes. “Give them all the information,” she said. “Make sure that you include the ‘why’ with all of this. Do not just start with ‘We need this built out now’ or ‘You need to tell me this or that.’ Go to the why. You do have to talk about the administration, about the [CMS health equity] pillars. To add those on to the front end really helps bring it into place of why it is overall important.”
“These are the conversations that were had on a system leadership level so that our leadership would be aware of the topic overall,” said Dr. Whiting. “As stated earlier, [this was] in relation to the possible need for additional FTEs, et cetera. This proactive approach was taken instead of the possibility of system leadership hearing about the influx of needs from case management departments later this year with no background of the health equity measures. The meeting with departments phase included meeting with system leadership and CNO/CQO representation from all of the hospitals.”
Take advantage of existing processes and resources.
External tools and resources that Houston Methodist already used were valuable during this time. Harrison and Dr. Whiting found that some features planned in their EHR’s forthcoming upgrade would be beneficial as they developed their screening tool. This saved several departments from duplicating efforts that were well thought through but needed to align with the CMS measures before implementation. This also reduced redundancies for end users of these processes.
Understand that this is an evolving process.
As teams work to address the new measures, they should keep in mind that some changes may be still to come. This is why Harrison emphasizes the importance of turning to existing resources and processes first, as opposed to making large investments in systems that may become less useful if additional guidance is released. “You do not want to put a lot of new processes in place right now if [CMS] is going to firm it up and change it a little bit next year,” said Harrison. “If you put all your energy, time, and money into a data collection tool or something, you may find out it is not what you need when the measures have more details.”
Learn as you go.
Facilities are sure to encounter obstacles as they work toward addressing these new measures—which is all the more reason why it is important to begin now and make adjustments along the way. “We have this year—the rest of this year until December—to kind of figure this process out, because these two [SDOH screening] measures are not required for 2024,” said Harrison. “This year is the year for us to figure it out and to really solidify a good process that we can build on.”
Conclusion
Advancing health equity does not happen overnight. As Houston Methodist demonstrated, working to meet the new CMS health equity measures is a lengthy process, involving careful planning and detailed workflow considerations. However, by collaborating with other departments, leaning on existing processes, starting small with a pilot program, and having the flexibility to adjust along the way, Houston Methodist is well on its way to continuing to incorporate a health equity focus throughout the health system in relation to the CMS measures.
These three measures are likely just the beginning. As the 2022 CMS Framework for Health Equity indicates, CMS has outlined a comprehensive, 10-year approach for embedding health equity throughout all CMS programs—which is sure to result in additional measures for participating hospitals in the coming years.
By taking action now, hospitals and health systems will ensure that they are prepared to not only meet the new measures but also further their ability to address health disparities and improve health outcomes for all populations in 2023 and beyond.